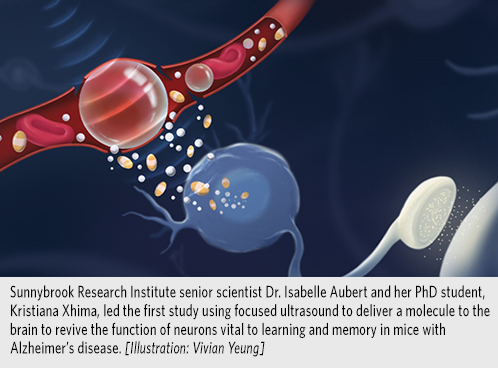
 The research team led by Isabelle Aubert, PhD, at Sunnybrook Research Institute (SRI) in Toronto, Canada, has successfully used focused ultrasound to permeabilize the blood-brain barrier (BBB) and deliver a compound that stimulates brain cell communication in mice with Alzheimer’s disease—potentially restoring neurons that are vital to learning and memory. The groundbreaking study was recently published in Science Advances.
The research team led by Isabelle Aubert, PhD, at Sunnybrook Research Institute (SRI) in Toronto, Canada, has successfully used focused ultrasound to permeabilize the blood-brain barrier (BBB) and deliver a compound that stimulates brain cell communication in mice with Alzheimer’s disease—potentially restoring neurons that are vital to learning and memory. The groundbreaking study was recently published in Science Advances.
In the brain, a molecule called nerve growth factor (NGF) promotes the survival, growth, and function of neurons. Alzheimer’s disease negatively affects NGF, and evidence has shown that simply restoring NGF to a damaged brain does not restore function. NGF binds to two receptors: tropomyosin receptor kinase A (TrkA), which activates a neuroprotective pathway, and p75 neurotrophin receptor (p75NTR), which can cause cell death and inflammation.
Uri Saragovi, PhD, at the Lady Davis Institute, Jewish General Hospital, McGill University, developed a compound, called D3, which could be of greater benefit than NGF because it uniquely binds to TrkA (pronounced “Track A”), and not p75NTR. To overcome the challenge of delivering D3 to the brain, Aubert and Saragovi teamed up with Senior SRI Scientist, Kullervo Hynynen, PhD, who was the first to show that focused ultrasound could locally, temporarily, and noninvasively open the BBB under MRI guidance.
In “Focused ultrasound delivery of a selective TrkA agonist rescues cholinergic function in a mouse model of Alzheimer’s disease,” the team, including first author and PhD student Kristiana Xhima, delivered D3 to the basal forebrain. After treatment, Xhima saw the first sign of success: TrkA was activated. She was excited to discover that TrkA stimulation by D3 enhanced the production and release of acetylcholine. The next step is to determine whether the compound improves memory—something the researchers are studying.
Focused ultrasound offers a safer and more precise way to deliver D3 than traditional methods such as intracranial injection. Importantly, D3 delivery restores communication between cholinergic neurons in the diseased brains. Cholinergic cells are essential for learning and memory. This could mean the technique could be used as a restorative therapy, especially at early stages of the disease.
For Dr. Aubert, the results achieved with the D3 molecule represent an exciting stride forward. She notes that clinical trials testing drugs that clear amyloid and tau have been disappointing, and that combining D3 with such a treatment could be an effective one-two punch. “Nothing has really panned out as being curative, to date. Alzheimer’s disease is complex. Sure, we have to get rid of the pathologies—including those related to amyloid and tau—but we have to help the brain function better. That’s where the neurofunctional components come in.”
Read Sunnybrook’s press release >
Read a Q&A with Aubert and Xhima >
Related Articles
Investigator Profile: Isabelle Aubert, PhD December 2019
Sunnybrook Centre of Excellence Accelerating Progress Through Collaboration November 2016
